There is a strange bit of silence that envelops the topic of pain during sex. Even though almost one in ten women in Britain experience painful sex at some point in their lives, many seem to assume that their bodies are just difficult or that everyone else is secretly dealing with the same thing. They are not.
Pain during intimacy, medically known as dyspareunia, is a clear sign that something in your body needs attention. While endometriosis in particular takes centre stage in these conversations, it is not the only explanation for the issue. With that in mind, let us examine some of these potential causes and explore what you can do to address this issue.
Why pain during sex should not be treated as normal
Let’s get one thing out of the door first: discomfort of any level during sex is not okay and should not be dismissed as usual. Not only that, but what matters most is understanding what your specific pain is trying to tell you. The devil is in the details. Whether it’s a sharp sensation deep inside, a burning feeling at the entrance, or an ache that lingers afterwards, each is a sign of an issue that requires prompt investigation. Some women tend to experience pain only with deep penetration. Others feel it right at the beginning or during periods. Some may even find it constant regardless of their cycle. These variations are all symptoms of different underlying causes, each with its own specific type of treatment. The location, timing, and quality of your discomfort are actually diagnostic clues that can guide your doctor toward the correct answer.
What are the possible causes of pain during sex?
Endometriosis
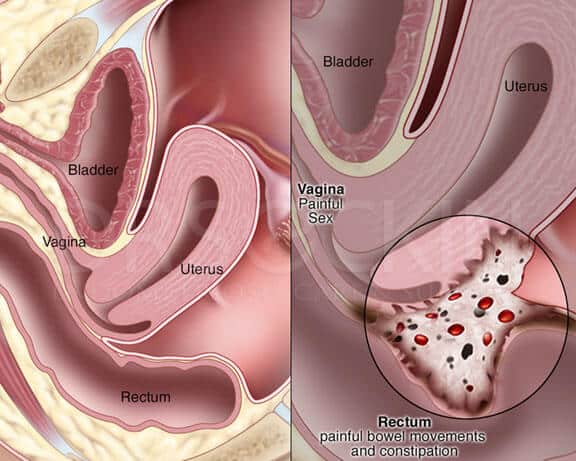
While this condition receives considerable attention on this topic, much of it is absolutely warranted. Endometriosis occurs when tissue similar to the lining of your uterus grows outside it, targeting your ovaries, fallopian tubes, or pelvic lining.
This misplaced tissue can cause deep pelvic pain, which peaks during menstruation. But endometriosis is only one piece of what is likely a much larger puzzle. We’ll discuss how to determine if it’s specifically your issue in just a moment.
Vaginismus
Vaginismus is an involuntary protective response wherein your pelvic floor muscles tighten automatically, making penetration difficult or impossible. This is a condition that tends to develop after trauma, arise from anxiety, or appear seemingly out of nowhere. The pain from vaginismus is generally felt at the entrance of the vagina, and it often feels like hitting a wall. Regardless of its origin, it is not something that can be consciously controlled or stopped. But with treatments like pelvic floor physiotherapy, you can have sex comfortably once more.
Pelvic Inflammatory Disease (PID)
PID is an infection that is usually caused by sexually transmitted bacteria spreading from your vagina to your uterus, fallopian tubes, or ovaries. Beyond making sex painful, its other symptoms include an unusual discharge, irregular bleeding, fever, and a persistent ache in your lower abdomen. Thankfully, this condition responds well to antibiotics when caught early. Left untreated, however, it can lead to complications, which makes getting checked sooner that much more important.
Other causes
Whether from hormonal changes, breastfeeding, menopause, or certain medications, vaginal dryness can make sex feel quite painful due to the increased friction. Then, infections like thrush or bacterial vaginosis can also cause inflammation and make the vagina sensitive to pain. There are also fibroids to be mindful of, which are non-cancerous growths that can cause a lot of pain depending on their size and location in the uterus. Hormonal fluctuations during your cycle can also cause issues in the reproductive system, leading to increased sensitivity in this area. What’s particularly problematic is that these conditions can coexist easily with one another. You could genuinely have endometriosis, but you might also be facing vaginismus at the same time, with both problems causing pain during sex. Once again, this is precisely why getting a thorough evaluation from someone who truly understands pelvic pain matters so much.
How can you tell if your pain is a sign of endometriosis?
When faced with pain during sex, you may have read about its relation to endometriosis, thinking that it must be the answer. However, as we’ve already established, this may not be the case, which is why you should consider consulting a private gynaecologist in London on this matter.
Endometriosis often exhibits distinct patterns that you should be aware of. The pain you feel might worsen just before and during your period. Many women with this condition experience painful periods that might feel more intense than a regular cramp, sometimes accompanied by pain that radiates to their back or legs. During sex, you might feel the pain deep inside your body, felt during or after penetration and with certain positions or angles. Some even say that the pain lasts up to 48 hours for them after sex.
The problem gets worse when you realise that not everyone with endometriosis experiences all these symptoms. You may struggle with endometriosis but experience minimal to no pain at all, while others might face a lot of pain from it.
When working with a doctor to figure things out, you may need to answer a few specific questions to help with their diagnosis. For example, when does the pain occur? Where exactly do you feel it? Does your menstrual cycle influence it? Have you noticed any other symptoms like heavy periods, fatigue, or digestive issues around your period?
Afterwards, they might also perform an internal examination, checking for tender spots or nodules that might suggest endometriosis. The gold standard for diagnosis remains laparoscopy, a minimally invasive surgical procedure that allows direct visualisation of your pelvic organs. Still, depending on your case, this may not be the first step.
However, if diagnosed, you will have several effective treatment options available that can improve your quality of life. Hormonal treatments can help manage the condition, there are a lot of pain relief strategies to provide comfort, and you always have surgical options at your disposal when needed. The right approach depends on your individual circumstances, symptom severity, and plans.
When should I seek help?
If possible, seek help immediately. There is no need to wait for the pain to become unbearable or for this issue to start affecting your relationships. Remember: Persistent pain during sex warrants a conversation with a healthcare professional. The sooner you do it, the better, as early intervention often prevents most of its potential causes from progressing and helps you return to comfortable intimacy more quickly.
Through a comprehensive assessment, a skilled gynaecologist will be able to accurately diagnose your specific case promptly. They’ll take time to understand your particular pain pattern, perform appropriate examinations, and arrange all the necessary tests for you to take as well. They will also be more than happy to coordinate care with other professionals if you need physiotherapy, pain management, or other specialist input. All that is to say: these specialists are there for you every step of the way, and they’ll make sure that you recover from this problem no matter what.
You deserve the best
Whether the cause behind your pain is endometriosis, vaginismus, an infection, or something else entirely, you must not accept it as normal or an inevitable part of being a woman. You deserve intimate experiences that feel good, not painful. At the same time, you deserve to be understood and properly diagnosed when faced with such problems. All that is required of you is letting go of any negative feelings associated with this pain and taking that first step towards finding the correct answers. Once you do so, everything will work out just fine.